The U.S. Chamber of Commerce’s attack on Rep. Bill Owens for supporting the Affordable Care Act is premised on misrepresentations of the law’s tax, spending, and Medicare provisions. In reality, the law expands services for seniors and provides tax credits to small businesses.
Many Small Businesses Are Eligible For Tax Credits Under The Affordable Care Act
Affordable Care Act Offers Tax Credits To Many Small Businesses. According to a report from Small Business Majority and Families USA: “Congress included in the Affordable Care Act a significant new tax credit for small business owners who provide their workers with health insurance. Under this new tax credit, businesses that have fewer than 25 full-time workers and average wages of less than $50,000 are now eligible to receive a tax credit of up to 35 percent of the cost of the health insurance that they provide for their workers. To qualify for the tax credit, small businesses must cover at least 50 percent of each employee’s health insurance premiums. In 2014, the size of the credit will increase to cover up to 50 percent of the cost of health insurance provided to workers.” [SmallBusinessMajority.org, May 2012]
- More Than 3.2 Million Small Businesses Eligible For ACA Tax Credit. According to a report from Small Business Majority and Families USA: “Our analysis found that more than 3.2 million small businesses, employing 19.3 million workers across the nation, will be eligible for this tax credit when they file their 2011 taxes. In total, these small businesses are eligible for more than $15.4 billion in credits for the 2011 tax year alone, an average of $800 per employee.” [SmallBusinessMajority.org, May 2012]
ACA Requires Businesses With More Than 50 Employees To Provide Affordable Coverage Or Pay A Fee. According to a report from Small Business Majority and FamiliesUSA: “While the Affordable Care Act created this new tax credit to help small business owners and workers, it does not force these small business owners to provide coverage for their workers. There are no employer mandates in the law, and there are no employer responsibility requirements at all for businesses with fewer than 50 workers, which account for 96 percent of all firms in the United States. Starting in 2014, businesses with 50 or more workers that do not offer coverage or that offer only unaffordable coverage to their workers will be assessed a fee if one or more of their workers receives a federal individual premium tax credit to purchase coverage in an exchange.” [SmallBusinessMajority.org, May 2012]
Rising Health Care Costs Are Due To Market Forces, And Are Slowed By ACA
Most Of The Rise In Insurance Premiums Is Due To Increasing Health Care Costs. From FactCheck.org: “Health insurance premiums for employer-sponsored family plans jumped a startling 9 percent from 2010 to 2011, and Republicans have blamed the federal health care law. But they exaggerate. The law — the bulk of which has yet to be implemented — has caused only about a 1 percent to 3 percent increase in premiums, according to several independent experts. The rest of the 9 percent rise is due to rising health care costs, as usual.” [FactCheck.org, 10/24/11]
Rising Health Care Costs Are Part Of A Long-Term Trend. The following chart from CNNMoney illustrates increasing health care costs between 2002 and 2011:
[Money.CNN.com, 5/11/11]
Without ACA, Health Care Costs Would Rise Even Faster. From CNNMoney: “The individual mandate would help spread health care costs to a larger pool of individuals, thus potentially lowering costs. Should the Supreme Court strike down the Affordable Care Act, consumers can expect that percentage to increase even more as costs rise ‘very fast,’ [Mathematica Policy Research senior fellow Deborah] Chollet said. Without the law’s measures to promote preventative care and spread costs across a larger population, overall costs will rise, she explained. Those without employer-provided health care coverage … will likely pay more for their plans because there will be fewer restrictions on insurers. Individuals could be denied coverage altogether because of a pre-existing health condition or offered coverage only at a very high premium, both of which are prohibited under the Affordable Care Act, Chollet added. Those with insurance through their employer will also pay more to cover the growing number of uninsured, she said.” [Money.CNN.com, 3/29/12]
Affordable Care Act Reduces The Deficit
CBO: The Affordable Care Act Will Reduce Deficits By Over $200 Billion From 2012-2021. According to Congressional Budget Office Director Douglas Elmendorf’s testimony before the House on March 30, 2011: “CBO and JCT’s most recent comprehensive estimate of the budgetary impact of PPACA and the Reconciliation Act was in relation to an estimate prepared for H.R. 2, the Repealing the Job-Killing Health Care Law Act, as passed by the House of Representatives on January 19, 2011. H.R. 2 would repeal the health care provisions of those laws. CBO and JCT estimated that repealing PPACA and the health-related provisions of the Reconciliation Act would produce a net increase in federal deficits of $210 billion over the 2012–2021 period as a result of changes in direct spending and revenues. Reversing the sign of the estimate released in February provides an approximate estimate of the impact over that period of enacting those provisions. Therefore, CBO and JCT effectively estimated in February that PPACA and the health-related provisions of the Reconciliation Act will produce a net decrease in federal deficits of $210 billion over the 2012–2021 period as a result of changes in direct spending and revenues.” [“CBO’s Analysis of the Major Health Care Legislation Enacted in March 2010,” CBO.gov, 3/30/11]
“Over $1 Trillion” Refers To Cost Of Insurance Provisions – Not ACA’s Impact On The Deficit
July 2012: CBO’s Updated Estimate For Cost Of ACA Insurance Coverage Provisions Is $1.168 Trillion. According to a Congressional Budget Office Report titled “Estimates for the Insurance Coverage Provisions of the Affordable Care Act Updated for the Recent Supreme Court Decision”: “CBO and JCT now estimate that the insurance coverage provisions of the ACA will have a net cost of $1,168 billion over the 2012–2022 period—compared with $1,252 billion projected in March 2012 for that 11-year period. That net cost reflects the following: Gross costs of $1,683 billion for Medicaid, CHIP, tax credits, and other subsidies for the purchase of health insurance through the newly established exchanges (and related costs), and tax credits for small employers. […] Those gross costs are offset in part by $515 billion in receipts from penalty payments, the new excise tax on high-premium insurance plans, and other budgetary effects (mostly increases in tax revenues stemming from changes in employer-provided insurance coverage).” [CBO.gov, July 2012, internal citations removed]
- July 2012 Report Affirmed Projection That ACA Will Reduce Deficits. According to a Congressional Budget Office Report titled “Estimates for the Insurance Coverage Provisions of the Affordable Care Act Updated for the Recent Supreme Court Decision”: “CBO and JCT have not updated their estimate of the overall budgetary impact of the ACA; previously, they estimated that the law would, on net, reduce budget deficits.” [CBO.gov, July 2012]
Affordable Care Act Savings Do Not ‘Cut’ Medicare Benefits
Affordable Care Act Reduces Future Medicare Spending, But “Does Not Cut That Money From The Program.” According to PolitiFact: “The legislation aims to slow projected spending on Medicare by more than $500 billion over a 10-year period, but it does not cut that money from the program. Medicare spending will increase over that time frame.” [PolitiFact.com, 6/28/12]
- CBO’s July Estimate Updates Medicare Cost Savings To $716 Billion. According to the Congressional Budget Office’s analysis of a bill to repeal the Affordable Care Act, repeal would have the following effects on Medicare spending: “Spending for Medicare would increase by an estimated $716 billion over that 2013–2022 period. Federal spending for Medicaid and CHIP would increase by about $25 billion from repealing the noncoverage provisions of the ACA, and direct spending for other programs would decrease by about $30 billion, CBO estimates. Within Medicare, net increases in spending for the services covered by Part A (Hospital Insurance) and Part B (Medical Insurance) would total $517 billion and $247 billion, respectively. Those increases would be partially offset by a $48 billion reduction in net spending for Part D.” [CBO.gov, 8/13/12]
GOP Plan Kept Most Of The Savings In The Affordable Care Act. According to the Washington Post’s Glenn Kessler: “First of all, under the health care bill, Medicare spending continues to go up year after year. The health care bill tries to identify ways to save money, and so the $500 billion figure comes from the difference over 10 years between anticipated Medicare spending (what is known as ‘the baseline’) and the changes the law makes to reduce spending. […] The savings actually are wrung from health-care providers, not Medicare beneficiaries. These spending reductions presumably would be a good thing, since virtually everyone agrees that Medicare spending is out of control. In the House Republican budget, lawmakers repealed the Obama health care law but retained all but $10 billion of the nearly $500 billion in Medicare savings, suggesting the actual policies enacted to achieve these spending reductions were not that objectionable to GOP lawmakers.” [WashingtonPost.com, 6/15/11, emphasis added]
Benefits For Seniors In The Affordable Care Act
Closing The Donut Hole
“Donut Hole” Is Gap In Drug Coverage For Annual Costs From $2,830-6,440. From CNNMoney: “What’s the donut hole? In addition to a $310 deductible, Medicare beneficiaries pay 25% of their drug costs until the total reaches $2,830 for the year. Then, they fall into a coverage gap. At that point, enrollees must pay all costs out of pocket until their annual expenses exceed $6,440. After that, seniors pay 5% of drug costs for the rest of the year. [CNNMoney, 6/7/10]
Affordable Care Act Eliminates Coverage Gap By 2020. The Kaiser Family Foundation explains how the Affordable Care Act closes the “donut hole”:
• In 2010, Part D enrollees with spending in the coverage gap will receive a $250 rebate.
• Beginning in 2011, Part D enrollees who reach the coverage gap will receive a 50 percent discount on the total cost of their brand-name drugs in the gap, as agreed to by pharmaceutical manufacturers.
• Over time, Medicare will gradually phase in additional subsidies in the coverage gap for brand-name drugs (beginning in 2013) and generic drugs (beginning in 2011), reducing the beneficiary coinsurance rate in the gap from 100 percent to 25 percent by 2020. [KFF.org, March 2010]
The Donut Hole Got “Noticeably Smaller” In 2011, Benefitting Over 2 Million Seniors. As the Associated Press reported: “Medicare’s prescription coverage gap is getting noticeably smaller and easier to manage this year for millions of older and disabled people with high drug costs. […] The average beneficiary who falls into the coverage gap would have spent $1,504 this year on prescriptions. But thanks to discounts and other provisions in President Barack Obama’s health care overhaul law, that cost fell to $901, according to Medicare’s Office of the Actuary, which handles economic estimates. […] More than 2 million beneficiaries already have gotten some help, discounts that have gone largely to middle-class seniors, because the poor are covered in the gap at taxpayer expense. [Associated Press, 11/27/11]
Expanding Preventive Care
Medicare Beneficiaries Receive Free Preventive Services, Annual Wellness Visits Under Health Care Law. As Kaiser Health News reported: “[T]he new health-care law will make it easier and cheaper for seniors to get preventive care. Medicare beneficiaries will be able to receive for free all preventive services and screenings that receive an A or B recommendation for seniors from the U.S. Preventive Services Task Force. That includes mammograms and colorectal cancer screening, bone mass measurement and nutritional counseling for people at risk for diet-related chronic diseases such as diabetes. Medicare beneficiaries will also get a free annual wellness visit under the new law. The visit will cover a number of services, including a health risk assessment and a review of the person’s functional and cognitive abilities. […] Currently, seniors in traditional Medicare pay 20 percent of the cost for most covered preventive services. [KaiserHealthNews.org, 8/10/10]
- More Than 25 Million Seniors Have Received Free Preventive Services. The Centers for Medicare and Medicaid Services reports: “According to preliminary numbers, at least 25,720,996 million Americans took advantage of at least one free preventive benefit in Medicare in 2011, including the new Annual Wellness Visit. This represents 73.3% of Medicare fee-for-service beneficiaries.” [CMS.gov, 2/15/12]
Health Insurers Poured Money Into Chamber To Attack Reform
Health Insurance Industry Gave Chamber Over $100 Million To Fight Health Care Reform. From the National Journal: “The nation’s leading health insurance industry group gave more than $100 million to help fuel the U.S. Chamber of Commerce’s 2009 and 2010 efforts to defeat President Obama’s signature health care reform law, National Journal’s Influence Alley has learned. During the final push to kill the bill before its March 2010 passage, America’s Health Insurance Plans gave the chamber $16.2 million. With the $86.2 million the insurers funneled to the business lobbying powerhouse in 2009, AHIP sent the chamber a total of $102.4 million during the health care reform debate, a number that has not been reported before now. The backchannel spending allowed insurers to publicly stake out a pro-reform position while privately funding the leading anti-reform lobbying group in Washington. The chamber spent tens of millions of dollars bankrolling efforts to kill health care reform.” [NationalJournal.com, 6/13/12]
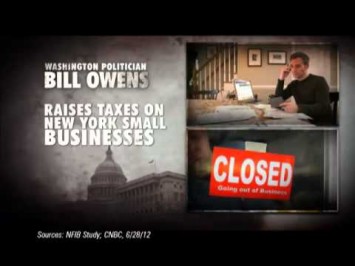
[Narrator:] Congressman Bill Owens is a typical Washington politician. Why did Congressman Owens help ram through government-mandated health care? The new health care law raises taxes and premiums on already struggling New York small businesses, adds over a trillion in new government spending, meanwhile, cutting $716 billion from Medicare. That hurts seniors. Congressman Owens voted for it. New York can’t afford Congressman Owens anymore. The U.S. Chamber is responsible for the content of this advertising. [U.S. Chamber via YouTube.com, 10/3/12]